Decay and Infections (Root Canals)
Back to: Clinical Team Procedures
CONDITION: Infections within a tooth
Root canal treatment is needed when either:
- A cavity is clinically into the pulp, or right up against it
- There is an irreversible pulpitis diagnosis
- There is a peri-apical radiolucency present.
If a tooth has a previous history of root canal treatment and the patient is asymptomatic, please consider that the radiolucency may be scar tissue and no treatment is needed. Compare prior xrays to determine if the lesion is improving, staying the same, or getting worse.
Also be aware, the mental foramen in the area of the lower premolars is often mistaken for a lesion.
If cavity excavation is right up against the pulp chamber, it has been our experience that these almost always lead to a root canal in the future. It is a better patient experience to simply perform or refer the root canal now, than to have them wait and it ‘blow up’ in pain surely on a Friday night. Try to have had this conversation that a pulp exposure is a possibility BEFORE YOU WORK ON THE TOOTH. Patients have a different perception of ownership of the problem if they were warned beforehand versus if they were told after the fact.
All posterior endodontically treated teeth need buildups and crowns. This is considered urgent treatment.
All anterior endodontically treated teeth can be restored via fillings or via crowns. As a general rule, if more than one interproximal surface needs to be restored a crown is recommended.
| Condition | Treatment Plan |
|---|---|
| Decay 80% to nerve radiographically | RCT |
| Irreversible pulpitis | RCT |
| Necrotic pulp | RCT |
| Posterior RCT | Crown & Buildup |
| Anterior RCT (M&D decay) | Crown |
| Anterior RCT (M or D decay, >50% tooth remain) | Buildup/Filling |
Pulp testing tip. We have found using the “cold test” for testing teeth vitality and to help with pulpal diagnosis to be the most reliable for of pulp testing. Below are general guidelines for how we pulp test.
-
Explain the situation to the patient. Mrs Jones, we are not trying to make you uncomfortable, we simply need to be sure we know which tooth is causing the problem here and what that tooth needs to be fixed properly. In order to figure this out, we need to test some teeth in this area with a cold stimulant. When we place cold on a tooth there are usually 3 possibilities that occur
-
You will feel the cold and as soon as the stimulus is removed the cold goes away in a few seconds. This means the tooth is healthy
-
You won’t feel the cold at all. This usually means the tooth is dead and is in need of root canal treatment or the pulp is so receded and protected by crown or filling material you simply cannot feel the cold
-
You will feel the cold, it will be uncomfortable and even after the cold stimulus is removed the ache sensation can linger for for some time. Unfortunately, this is a sign that the nerve is in the process of dying. A root canal is indicated.
-
2. Test the contralateral healthy tooth first (if not RCT treated already). Dry the tooth and place the cold on the tooth. Tell the patient to raise their hand when they feel the cold and then remove the stimulus. Then ask the patient to let you know when the cold has fully gone away. It should be less than 10 seconds. Using “endo ice” refrigerant spray, Its best to use a loose cotton pellet being held by a cotton forceps. A tightly wound Q tip is not as predictable.
3. Test teeth mesial and distal to the suspected tooth
4. Test the suspected tooth
5. Be aware some people have very hyper sensitive teeth. If all their teeth linger for 10s this does not mean they all need root canals. Look for the problem tooth to be significantly more intense and/or linger longer.
| Reaction From Cold | Diagnosis | Treatment Plan |
|---|---|---|
| Sharp, gone in 10s or less | Healthy Pulp | Restorative If Needed |
| No Reaction | Pulpal Necrosis | RCT |
| Ache, delayed onset, lingering when compared to other teeth | Irreversible pulpitis | RCT |
Lower molar with cavity into the pulp. This patient was diagnosed with irreversible pulpitis.
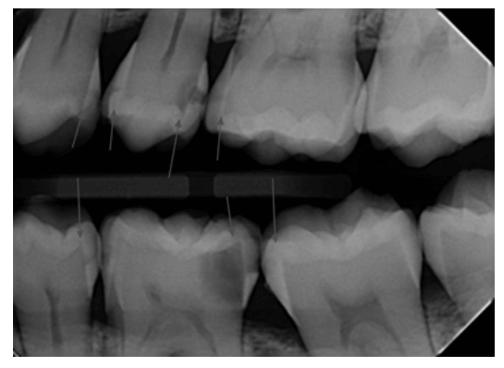
Active abcess on both roots. Root canal treatment is indicated here.

